Introdução
Dra. Tatiana Tournieux
Nós, médicos, sabemos que em qualquer tratamento é preciso pesar os prós e os contras. Não devemos esquecer Hipócrates, o pai da medicina ocidental, que proferiu o aforismo: “Primum Non Nocere”, ou “primeiro não causar dano”.
Sendo assim, seria ideal que todos os cirurgiões ou serviços olhassem para trás e avaliassem seus casos.
Infelizmente, publicações com esse foco ainda são pouco frequentes.
Por este motivo, neste momento, optamos em republicar um trabalho de autoria de Sandro Salanitri, juntamente com Antonio José Gonçalves, Américo Helene, Jr. e Flavia Helena Junqueira Lopes, que fazem uma análise crítica das possíveis (embora felizmente infrequentes) complicações na cirurgia de transplante capilar e assim servir de exemplo e também referência para todos nós.
_______________________________________________________________________
Surgical Complications in Hair Transplantation: A Series of 533 Procedures
Sandro Salanitri, MD, Antonio José Gonçalves, PhD, Américo Helene, Jr., PhD, Flavia Helena Junqueira Lopes
Aesthetic Surgery Journal, Volume 29, Issue 1, January 2009, Pages 72–76,
https://doi.org/10.1016/j.asj.2008.11.005
Published: 01 January 2009
Abstract
BACKGROUND: Surgical complications in hair transplantation can sometimes be a serious matter. Most of the published literature on this issue deals with individual case reports rather than larger series of patients.
OBJECTIVE: The authors analyze complications in 425 consecutive patients undergoing 533 hair transplantations.
METHODS: Patients with androgenetic alopecia (407 men and 17 women), cicatricial alopecia (9 men and 8 women), and malformations (1 man and 3 women) with a mean age of 36.9 years (standard deviation, 10.4 yrs) underwent hair transplantation between 1995 and 2006 and were followed up postoperatively for at least 1 year. Data on surgical complications were retrospectively analyzed.
RESULTS: The overall complication rate in our series was 4.7%, including enlarged scar (1.2%), folliculitis (1.0%), necrosis in the donor area (0.8%), keloids (0.4%), bleeding (0.2%), hiccups (0.2%), infection (0.2%), and pyogenic granuloma (0.2%). The frequency of enlarged scar increased proportionally according to the number of surgical procedures.
CONCLUSIONS: The hair transplantation complication rate in this series was 4.7%. Good communication between patient and surgeon, a complete clinical and laboratory assessment of the patient, accurate surgical technique, specific equipment, a trained surgical team, and careful postoperative attention to the patient are crucial for successful hair transplantation and for decreasing complication rates.
Hair transplantation has often been used for the aesthetic correction of baldness. More than 225,000 hair transplantations are carried out every year worldwide. Although isolated cases of aesthetic and medical complications in hair transplantation have been reported, publications of larger series in the literature have been lacking. Inappropriate surgical indications or inadequate communication between patient and physician are generally responsible for aesthetic complications, although obsolete or unorthodox techniques may also lead to unsatisfactory results.
Reports of isolated hair transplantation cases have focused on complicating factors, such as persistent hiccups,2–6 von Willebrand disease, hereditary angiodema,7 herpes zoster,6 and malignant hyperthermia,3 all manifesting themselves during or after hair transplant. Complications of the procedure have included alterations in scars (cobblestoning, riding [elevation of skin in the transplanted area], and various degrees of fibrosis and/or keloids),8 pigmentation disturbances, hair kinking (deformity of the hair post–hair transplant),9 arteriovenous fistulas,10–15 dehiscence, scar enlargement and necroses (described in donor and in receptor and donor sites),3, 5, 6, 16–18 areas of postoperative folliculitis,19 scalp infection, and osteomyelitis of the cranium.20
In this paper, we sought to determine both the type and frequency of complications in a series of 533 hair transplantations and discuss their prophylaxis and treatment.
Methods
This retrospective study, approved by the Ethical Committee of the Medical School of the Santa Casa de São Paulo, included data from 445 patients (mean age, 36.9 ± 10.4 yrs) who underwent a total of 533 surgical hair transplantation procedures at the Plastic Surgery Division of Santa Casa de Misericórdia de São Paulo or in a private clinic from February 1, 1995 to January 1, 2006.
Most of the patients were men (93.7%) with a mean age of 36.2 years ± 9.7 years. Women (6.3%) had a mean age of 47.8 years ± 18.7 years. Whites accounted for 90.3% of cases, followed by blacks (7.6%) and Asians (2.2%).
Reasons for hair transplantation included androgenetic alopecia in 424 patients (95.3%), cicatricial alopecia in 17 patients (3.8%), and malformations in 4 patients (0.9%). Both cicatricial alopecia and malformations were more frequent among females (39.5%), while most males (97.6%) presented with androgenetic alopecia. Blacks presented with cicatricial alopecia more often frequently than whites or Asians.
Hair transplantations were performed in the scalp only (98.9%), moustache (0.7%), and scalp and eyebrows (0.4%). One surgical procedure sufficed for 373 patients; 2 procedures were necessary for 61 patients; and 3 procedures were performed in 7 patients. Four patients underwent 4 surgical procedures, and 5 procedures were necessary in one case.
Surgical Technique
Sedation was administered using midazolam and fentanyl. Troncular local anesthesia with xylocaine and marcaine was administered without constriction, followed by the infiltration of saline solution and adrenaline 1:150,000 in both the donor and receptor areas. In the ventral position, epilation and preoperative markings were performed in the donor area (defined as about 22 cm in length and 2 cm in width at the height of the occipital protuberance). A beveled incision was made in the donor area of the scalp, respecting the topography of the piloses follicle, followed by dissection of the donor area above the subcutaneous fat, hemostasis of the lower plane, and continuous suture with 3.0 nylon sutures. Dissection of the follicular units and follicular families of 2 to 5 follicules was performed using stereoscopy and a light table. The hydrate follicles were maintained in a 0.9% saline solution chilled at 4°C. With the patient in the dorsal decubitus position with the head elevated, the transplantation of the follicles and the follicular families was accomplished in the frontal and temporal regions using a No. 15 Beaver blade, and in the occipital area using a No. 11 Beaver blade, by means of the surgical technique of stick and place, followed by clean-up and placement of an occlusive bandage.
All patients received postoperative antibiotic therapy, intramuscular corticoids, and analgesic medication. Bandages were kept on for 1 day. Patients were followed up in the immediate postoperative period, at 3, 7, and 14 days, and then monthly up to 1 year postoperatively. Occasionally, if necessary, an additional transplantation session was carried out after at least 8 months follow-up.
Quantitative data were analyzed with ?2 and Fisher tests and analysis of variance (ANOVA). Mann–Whitney statistics were used for quantitative and qualitative analysis with a significance of 5% (P < .05).
Results
Complications were observed in 21 patients (4.7%) in a total of 27 procedures (5.0%), as shown in the Table. Black patients developed complications more frequently than whites (12.1% and 4.5%, respectively), but this difference was not significant (P = .094). Most complications (95.6%) were observed in scalp hair transplantation procedures. Infection developed in 1 black patient after moustache hair transplantation. Patients who underwent only 1 procedure developed an average of 1.17 complications, which was significantly lower (P = .003) than the average number of complications (1.67) in patients who underwent more than 1 session.
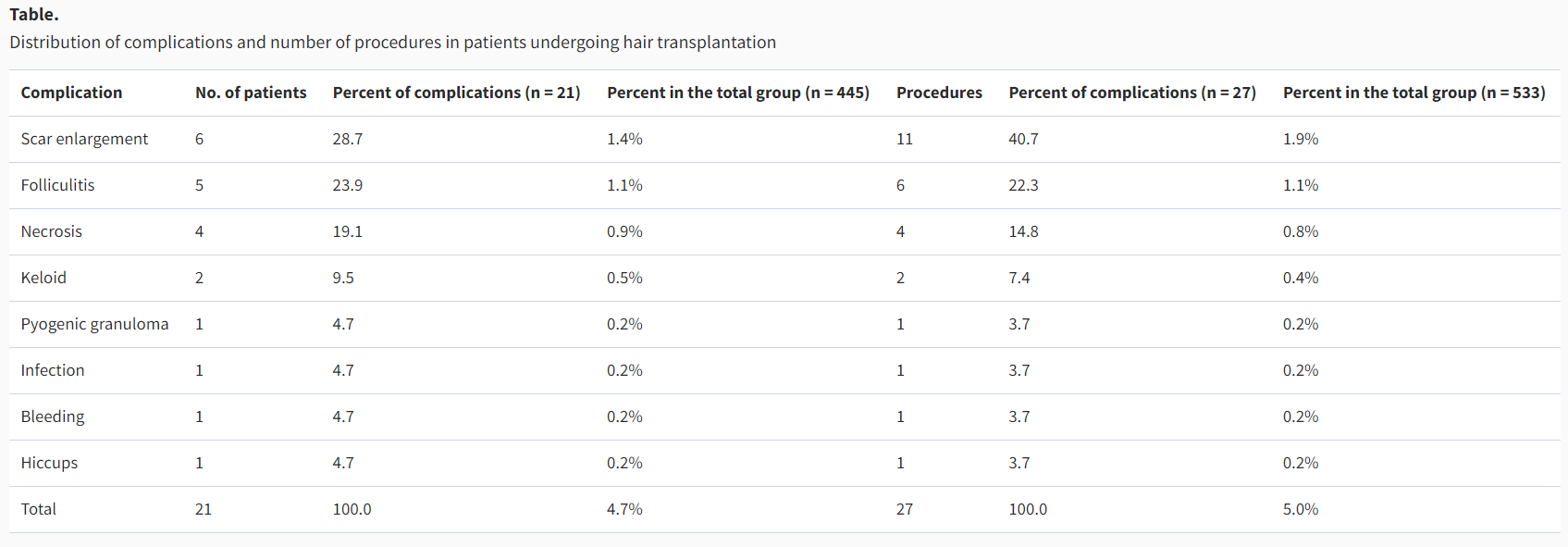
Complications were observed in 13 of the 337 patients who underwent only 1 procedure. One patient who underwent 2 procedures presented with folliculitis after each of them. Another patient who underwent 3 procedures presented with folliculitis only after the third procedure. Scar enlargement was observed after an initial procedure in 2 cases. Two patients who each underwent 2 procedures presented with scar enlargement after both procedures. Scar enlargement was also observed after the third and forth procedures in a patient who had 4 treatment sessions and after the third, fourth, and fifth procedures in another patient who had 5 treatment sessions. Finally, bleeding was observed on the second postoperative day after the first session in a patient who underwent 2 procedures.
Discussion
Hair transplantation has been considered to be a simple surgical procedure with minimal complications rates.4 However, there is a large variety of possible complications, although some of them are not widely known and some surgeons may fail to recognize them.5, 18, 21
In recent years, only a few studies have reported on the type and frequency of complications occurring in large patient series. Instead, most of the literature deals with cases involving one specific complication or another. Older studies17 and standard texts16, 18 report a very low incidence of hair transplantation complications,16, 18 especially when compared to other procedures in plastic surgery.6 We observed a higher complication rate of 4.7%, perhaps because these earlier studies dealt with only medical complications directly related to the transplantation while ignoring aesthetic complications.
Similar complication rates were observed among men and women and in the different alopecia cases. Black patients presented with complications more frequently than whites or Asians. Although the difference was not statistically significant, it would be worthwhile to conduct a study that included a patient series with a larger black population.
Scar enlargement (Figure 1) was the main complication encountered in our series, accounting for 25.9% of complications. Enlargement occurred despite the use of longer and narrower resections in the donor area (maximum, 2 cm) which resulted in a less tensile suture. We believe individual idiosyncrasies—with respect to skin elasticity, number of follicles, and the number of previous resections in the donor area—all played a role in the quality of the scar. In some cases, it was easy to suture the donor area without placing pressure on the borders even after 3 procedures, while in others, suturing was difficult after only 1 procedure. Nonetheless, it is not necessarily the case that more tensile sutures cause scar enlargement. Additional studies are needed on the individual factors that may be associated with a predisposition to scar enlargement. Our results also indicate that performance of additional procedures in the same patient was linked to a higher incidence of scar enlargement. Two black patients presented with keloids (Figure 2), which in our opinion represent an important complication that is difficult to treat successfully. In 1 case, the complication involved the donor area and was successfully managed with corticoid therapy, intralesional resection, and radiotherapy. In the other case, the receptor area was involved and was successfully treated with corticoid therapy. Blacks are reportedly more predisposed to the development of keloids.8

Scar enlargement in a 35-year-old man 1 year after surgery.

Keloid in a 40-year-old man 11 months after surgery.
The second and more frequent complication encountered in this series was folliculitis (22.3%). It is an unusual complication after hair transplantation that occurs more frequently in patients with very curly hair and in black patients, who in fact are likely to develop folliculitis (Figure 3). Proper graft placement in the donor area is crucial to minimize the incidence of folliculitis, but the perfect placement of all the grafts (1000 per session, on average) without burying any of them at the end of the procedure and following bandage removal can be technically very difficult. Folliculitis was observed in the majority of our patients.19 Unger18 reported a folliculitis rate of 20% of his study group. Our rate is higher, which we believe reflects individual idiosyncrasies among our patient group. Treatment involved administration of tetracycline throughout the hair-growing period. We recommend the use of antibiotic therapy before and after any required additional procedure in such cases.

Folliculitis in a 25-year-old man 11 months after surgery.
Necrosis (Figure 4) was observed in 4 patients (1.4% of complications). In 3 cases caused by local trauma, only a small area of the scalp was involved (average, 1 cm diameter). One case involved a 3-cm diameter necrosis in the central occipital area, associated with expulsive grafts and consequent local alopecia. It was treated with a new grafting immediately after cicatrization. Because the donor area anesthesia lasts for an indeterminate amount of time and patients can sometimes be negligent, daily activities such as getting out of a car or walking under a low passageway or ceiling can lead to generally small local traumas that resolve spontaneously. Smokers and diabetic patients tend to bleed less during surgical procedures, which can signify a microvascular disorder. Consequently, a rigorous preoperative assessment and abstinence from smoking for at least 30 days before and 30 days after surgery are recommended. Circulation in the scalp is marginal and without perforating veins in any event; moreover, vascularization is further diminished in patients with androgenetic alopecia.22 In our series, necrosis always occurred in the central occipital area, that is, the least vascularized scalp area. Transection in any vessel in the supragaleal plexus can also result in necrosis. Hair transplantation should be avoided in patients with vascular supply deficits.

Scalp necrosis in a 30-year-old woman 1 month after surgery.
In the case of 1 patient who presented with pyogenic granuloma (Figure 5), we used a wood plaque for dissecting the grafts, and it probably released immunogenic wood microfragments that produced local foreign body granulomas. We have been preventively using polyvinylchloride (PVC) plaques, which are less immunogenic. Management for this complication focuses on local curettage and removal of all the microfragments.

Pyogenic granuloma in a 26-year-old man 6 months after surgery.
Infection was observed in moustache hair transplantation in 1 patient who had a cold and who removed the curative before the recommended period. Development of local cellulitis was successfully managed with antibiotic therapy, but with partial loss of the grafts. Infection cases reported in the literature usually were associated with immunity deficits, diabetes, or postoperative hygienic negligence. Unger18 reported an incidence of 0.1% in such cases. Some authors are concerned about infection in hair transplantation, but others understand it as a clean surgery that does not require antibiotic prophylaxis. It is important to note, however, that severe skull osteomielitis after hair transplantation has already been reported in the literature.20 We believe that infection is actually a rare but severe complication that can be avoided by the use of adequate local asepsis and antisepsis and antibiotic therapy.
Bleeding in the immediate postoperative period occurred in 1 patient and was effectively treated by local compression for 10 minutes. Bleeding in the donor area seems to be a frequent complication18 but is observed less frequently in the receptor area. Very excited or hypertensive patients can experience postoperative bleeding.17
Limited hair growth after transplantation can be the result of the surgical procedure or can be related to idiopathic factors. The surgical causes, or X factor, include inadequate dissection of the grafts, inadequate stockage, the use of very large grafts, and the close placement of many grafts. Idiopathic causes include hypertension, diabetes, and smoking. Some individuals can also experience limited hair growth in the central area of the scalp versus other peripheral areas because of the relative hypovascularization in the central area. Rarely, genetic predisposition to limited hair growth after transplantation independently of the employed surgical technique may be present.23
Graft growing failed almost completely in 2 black patients. It was not considered a complication because it seemed a technical deficit that could be solved with better dissection, one that takes the features of very curly hair follicles more into account, because they exhibit an indeterminate implantation pattern that requires special care in dissection. Postoperative care must be rigorous in such patients, including shorter follow-up intervals in order to search for hairs tending to become ingrown because of the curvature of their roots in order to exteriorize them, minimize the risk of folliculitis, and achieve better results.
Hiccups developing immediately after the procedure and lasting about 48 hours were observed in 1 patient and were managed with metochlopramide. Hiccups are common during hair transplantation because of the patient's dorsal placement. They can also result from excessive air aspiration consequent to stimulation of diaphragmatic muscle movements by very excited or vocal patients.2
Postoperative edema is reportedly a common complication, especially when larger grafts are used.11 Its severity hinges on the number of transplanted grafts, duration of the session, and genetic factors. It is usually observed in the infra- and supraorbital areas after placement of the frontal capillary line between the second and the fourth postoperative day. Pain and discomfort 24 to 48 hours postoperatively have also been reported. “Discomfort” generally refers to a severe headache resulting from inadequate local anesthesia.9 We do not consider some level of edema, pain, and/or ecchymosis to represent a complication but regard it instead as an organic and individual tissue response to the trauma.
Conclusions
Successful hair transplantation and a decreased rate of complications depend on good communication between surgeon and patient, careful clinical and laboratory evaluation of the patient, carefully selected technique, specific equipment, a trained surgical team, and rigorous postoperative evaluation. We believe that our findings can contribute to increased awareness of the types and frequency of hair transplantation complications, and will stimulate more rigorous studies on this issue so that clinical practice and surgical techniques for the management of alopecia can be further improved.
Disclosures
The authors have no disclosures with respect to the contents of this article.
References
1.ISHRS 2007 Practice Census Facts and Figures. International Society of Hair Restoration Surgery. Available at http://www.ishrs.org/mediacenter/pr/pr12a.html. Last accessed January 16, 2009.
2.Arnold J Hiccups following surgery of the scalp. Complications In: Stough DB Haber RS, editors. Hair replacement St. Louis: Mosby 1996:332–334.
3.Beeson WH Emergency situations in hair transplantation In: Stough DB Haber RS, editors. Hair replacement St. Louis: Mosby 1996:334–340.
4.Marzola M Vogel JE Complications In: Haber RS Stough DB, editors. Hair transplantation Philadelphia: Elsevier Saunders 2006:257–283.
5.Stough DB Randall JK Schauder CS Complications in hair replacement surgery Facial Plast Surg Clin North Am 1994;2:219–229.
6.Uebel CO Complications and undesirable results In: Webel CO, editor. Hair restoration micrografts and flaps Porto Alegre: OESP Grafica S/A 2001:297–323.
7.Jackson BD Stough DB Hereditary angioedema and hair restoration surgery In: Stough DB Haber RS, editors. Hair replacement St. Louis: Mosby 1996:341–342.
8.Randall JK Stough DB Scarring and keloid development after alopecia correction surgery In: Stough DB Haber RS, editors. Hair replacement St. Louis: Mosby 1996:323–326.
9.Sadick NS Hashimoto KN Anatomical hair shaft sequelae of hair transplantation complications In: Stough DB Haber RS, editors. Hair replacement St. Louis: Mosby 1996:316–320.
10.Barros d'Sa AA Heard CE Arteriovenous fistula after hair transplantation Br Med J 1978;1:340–3411.
11.Nordström REA Saara T Iatrogenic false aneurysms following punch hair grafting Plast Recontr Surg 1979;64:563–565.
12.Norwood OT Arteriovenous fistula resulting from hair transplantation Cutis 1970;6:263–264.
13.Semashko DC Schwartz ME Kaynan A Harrington EB Arteriovenous fistula following punch-graft hair transplantation J Dermatol Surg Oncol 1989;15:754–755.
14.Souder DE Bercaw BL Arteriovenous fistula secondary to hair transplantation N Engl J Med 1970;283:473–474.
15.Weideig JC Arteriovenosus malformation after hair transplantation In: Stough DB Haber RS, editors. Hair replacement St. Louis: Mosby 1996:299
16.Buchwach K Konior RJ Complications In: Buchwach K Konior RJ, editors. Contemporary hair transplant surgery New York: Thieme 1997:151–169.
17.Stough DB Complications of hair transplantation Cutis 1970;6:645–651.
18.Unger WP Complications of hair transplantation In: Unger WP, editor. Hair transplantation3rd ed. New York: Dekker 1995:363–374.
19.Whinting DA Stough DB Posttransplant epidermoid cysts secondary to small-graft hair transplantation In: Stough DB Haber RS, editors. Hair replacement St. Louis: Mosby 1996:320–323.
20.Jones JW Ignelzi RJ Frank DH Blackock JB Osteomylitis of the skull following scalp reduction and plug transplantation Ann Plast Surg 1980;5:480–482.
21.Swinerhart JM Complications, repairs and special situations In: Swinerhart JM, editor. Hair restoration surgery Stamford, CT: Appleton & Lange 1996:355–370.
22.Klemp P Peters K Hansted B Subcutaneous blood flow in early male pattern baldness J Invest Dermatol 1989;92:725–726.
23.Shiell RC Poor hair growth after hair transplantation: the x factor In: Stough DB Haber RS, editors. Hair replacement St. Louis: Mosby 1996:314–316.
Folículo - Edição 24